










WORLD CLINICAL PATHOLOGICAL CASE (CPC) COMPETITION
The Clinical Pathologic Case (CPC) competition is one of the highlights of WACEM. CPC is a fun and instructive way of demonstrating the “emergency medicine approach” to the diagnosis and initial management of patients with undifferentiated complaints. The best CPC cases are either unusual presentations of common diagnoses, or common presentations of unusual diagnoses.
There are two main components to the CPC competition: (1) the case presentation, and (2) the case discussion. The case presentation is an opportunity to for Faculty to demonstrate their skill in performing a concise yet meaningful review of the pertinent historical, physical examination, and diagnostic approach to a complex Emergency Medicine case. The case discussion is opportunity for EM Residents to demonstrate their skill in developing a logical, deductive reasoning process used in clinical Emergency Medicine to arrive at the most probable diagnosis.
This document provides an in-depth look at what makes a truly great CPC case presentation, and how to develop an award winning case discussion. Both aspects of the CPC competition will take time, thought, and preparation to develop. Best of luck, and let the games begin!
Contest Rules
To enter the competition, each team must agree to provide a CPC case to the conference organizers on or before the Case Submission Deadline on 13TH NOVEMBER 2021 @ midnight (0:00) EST.
The rule is: each team must “give a case to get a case.” Any team that fails to submit a case by the Case Submission Deadline will forfeit their registration and be excluded from competition.
The conference organizers will review each case submission before assigning it to another team for analysis and preparation of discussion. Submissions must adhere to the selection and formatting guidelines provided below, and must clearly indicate the names, affiliations, and contact information of the submitting team members. The CPC organizers will work with each team to edit and improve their submission before final acceptance and assignment to another team.
TEAMS FORMATION:
Teams are composed of two people: one Faculty (case presenter), and one Resident (case discussant). Both team members must present at the competition. Faculty will present the case his/her team submitted. The Faculty presentation is in two parts: the case summary, and the case follow-up. The Resident will present his/her discussion of the case his/her team received. Faculty members are expected to provide mentorship and review their Resident’s case discussion.
Submission Rules
All submissions should be sent to wacemcpc2021@gmail.com All submissions MUST be in format below with WORD file labelled as CPC XYZ Institution.
The submission must include:
(1) name, title, and institutional affiliation of BOTH the resident and faculty preceptor who will present;
(2) the final diagnosis (for judges viewing only);
(3) proper email contact information for both resident and faculty teams; and
(4) a word document formatted as per rules describing the salient features of the case.
Please see the section on Case Selection and Presentation for more details on format for submission.
THE FINAL DEADLINE FOR SUBMISSION IS SATURDAY, 13TH NOVEMBER 2021 @ midnight (0:00) EST.
Please do well to submit early if possible. The judges will review all submissions before re-distributing to the teams and may contact you if questions arise as to formatting or presentation. Remember, we want cases that are both challenging and ultimately “solvable”!
Time Allotments for Presentations
Faculty Case Presentation: 4 minutes
Resident Case Discussion: 10 minutes
Faculty Case Follow-up: 4 minutes
Note: These are the maximum time allotments allowed for each segment of the CPC competition. Time limits will be strictly adhered to. Presentations that run over the allotted times will be stopped by the judges.
Special considerations for online-only CPC during the pandemic (ZOOM rules)
1. Video should always be on while you are presenting. Video may be paused when not actively speaking during the session.
2. Participants should also be mindful to mute themselves when not presenting.
3. A schedule for the order of presentations will be sent out to all participants before the session. The schedule will include times for breaks/lunch.
4. All participants must be logged in for the entire CPC competition.
5. If there are technical challenges with a speaker’s internet connection during a presentation, the judges may ask another team to present outside of their scheduled time slot. This is to prevent extended delays due to technical difficulties.
6. If technical problems with the connection prevent anyone from completing their presentation, they will be given an opportunity to complete it at the end of the session.
7. Judges will contact participants via the chat function to advise them of their turn if the schedule needs to be adjusted due to technical difficulties. If they do not respond, then they will be disqualified.
CHECK YOUR EMAILS REGULARLY SPAM AND INBOX FOR QUERIES AND COMMUNICATIONS FROM AND WITH THE JUDGES.
Case Selection and Presentation
1. SELECTING A GREAT CASE FOR SUBMISSION
The best CPC cases share three key elements: “relevance”, “solvability”, and “discuss-ability”.
Cases are considered relevant to emergency medicine practice if the final diagnosis can be deduced from information available during the ED evaluation. If the final diagnosis was confirmed later, or by a test not usually performed in the ED, enough information must be available at the time of ED presentation to place the diagnosis at the top of the list of probable diagnoses.
Cases are solvable if there is enough information to give the discussant a reasonable opportunity to make, deduce, or highly suspect the final diagnosis. Cases that are highly complex, contain multiple primary diagnoses, or are laden with extraneous facts may be impossible to solve. These are not good CPC cases.
Cases are discuss-able if they are challenging enough to require consideration of a reasonably broad differential diagnosis. Cases that are too “easy” or that contain clearly pathognomonic findings may not allow full demonstration of the logical, deductive process used to develop a thoughtful strategy.
2. PREPARING THE CASE FOR SUBMISSION
All case submissions must be sent electronically via email as Microsoft Word documents using the templated format provided below (see Appendix 1). Submissions sent in PPT or other formats will be returned to the team for reformatting before they can be considered.
Case submissions must include: chief complaint, history of present illness, pertinent past medical, surgical, social and family history, medications, allergies, physical examination findings, and selected diagnostic test results obtained in the emergency department (in that order). Avoid the use of abbreviations.
If possible, include photos or photocopies of electrocardiogram or radiographic studies. Be sure to remove any patient identifiers (such as patient name, date of birth, etc)! Do not interpret the data. If the images are of sufficient quality, let the discussant interpret the ECG, XR, or calculate the anion gap.
It is customary to present all information obtained in the ED, usually in the order in which it was collected. Let the discussant decide which bits of information are relevant and which are “red herrings”. Incomplete and irrelevant historical and physical examination data are part of the practice of Emergency Medicine. It may sometimes be appropriate to withhold a confirmatory test result obtained in the ED to improve “disscuss-ability”, as long as the case is still “solvable”. Remember, the goal of this academic exercise is not to “stump” the discussant, but to encourage a thoughtful discussion.
3. PRESENTING AND DISCUSSING THE CASE DURING THE COMPETITION
The Faculty case presenter will begin each case with a brief presentation of all information that was submitted. Do not provide any information to the audience that has not already been submitted to the discussant. Do not interpret data for the audience. Present the case, clearly,
concisely, and succinctly. Conclude the case presentation and offer the floor to the discussant. This should take no longer than four minutes.
After the Faculty presenter is finished, the Resident from the team who received the case will have 10 minutes for discussion. The discussion must conclude with a final diagnosis. You must pick one “best educated guess” based on the analysis of pertinent positives, negatives, and differential diagnosis. General tips on how to approach this discussion are provided below (see Appendix 2).
The Faculty case presenter then will provide a brief follow-up presentation (four minutes maximum). The goal is to reveal the final diagnosis, present any confirmatory diagnostic data, and provide 1-2 discussion points that explain the key features that should have pointed to the answer. A brief description of the patient’s hospital course and outcome is also appropriate here.
CHECK YOUR EMAILS REGULARLY SPAM AND INBOX FOR QUERIES AND COMMUNICATIONS FROM AND WITH THE JUDGES.
Appendix 2. TIPS FOR DESIGNING AN EXCELLENT CASE DISCUSSION
1. Understand the Goals of the CPC
The main goal of the CPC is to illustrate the logical progression from an undifferentiated emergency patient presentation to a narrowed differential diagnosis and focused management plan. This is your chance to demonstrate a rigorous, thoughtful approach to interpretation and analysis of (often confusing and incomplete) information. Do not get too caught up in making the correct diagnosis. Focus on the process by which a final diagnosis and evidence based management plan might be arrived at.
Discussing an unknown case in front of an audience can be stressful, but it is also exciting and challenging. Adequate preparation will make the presentation most enjoyable for you and for the audience.
2. Work through the case systematically
Start by reviewing the case. Initially, you should consider each data point that was given to be potentially relevant to the case resolution. Seemingly inconsequential information may prove to be pivotal. Next, think about which features of the case seem the most relevant. These salient features may include historical and physical data, diagnostic data, and the interpretation of diagnostic data. Each salient feature prompts a differential diagnosis. Consider a complete differential diagnosis for each feature. “If you don’t think of it, you’ll never diagnose it.”
After listing all the potential diagnoses, begin to narrow the list. As in clinical medicine, one of two approaches often leads to a reasonable approximation of the final diagnosis. The first approach is to recognize the data as part of a syndrome. A syndrome is a constellation of signs, symptoms and diagnostic data related to another by some anatomic, physiologic or biochemical abnormality. Compare the differential diagnosis lists developed for each salient feature with each other. Occasionally, a common thread, or syndrome, is discovered. The table below illustrates this process:
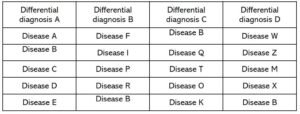
In this example, diagnosis “B” is on each list and may represent a syndrome. Most cases will not be so straightforward. Disease “B” may not be contained on every list or a second syndrome may be common to many lists. When more than one syndrome is possible, weigh each diagnostic possibility with respect to the presence of “syndrome defining” features. Successive approximation will suggest that one diagnosis is more probable than another is.
The second approach weighs each potential diagnosis in terms of supporting or refuting data. Create a differential diagnosis list for each salient feature. Compare each list to find diseases common to one or more of them. The second example illustrates this process:
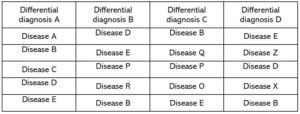
In this example, diseases “B” and “E” are on every list, disease “D” is on three lists, and disease “P” is on two lists. All other diseases are found only one time. The diseases common among several lists represent the most probable diagnoses. Consider clinical and diagnostic data that increases or decreases the probability that a diagnosis is correct. This table illustrates that process:
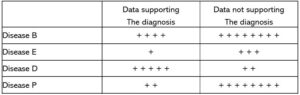
In this example, disease “D” seems more probable than other diseases. Although disease “B” and disease “E” appeared on every list, the weight of the data does not make the diagnosis probable. Some data is more specific and may weigh more than other softer data. The discussant logically weighs each potential diagnosis in terms of the data available to estimate a probability. The most probable diagnosis will be at the top of the final differential diagnosis list, the least probable at the bottom.
3. Prepare your CPC discussion slides
Various presentation formats are effective. Choose a presentation format that most suits your own thought process and communication style. The presentation format for the discussion could follow this general outline:
Review the salient features – suggest which items might be pertinent positives or negatives
List complete differential diagnoses for the salient features
Logical discussion of the potential diagnoses – pros and cons
Suggest the most likely diagnoses in a narrowed differential diagnosis list
Discuss studies or maneuvers you might use to make the final diagnosis
Arrive at your final, best educated guess of the final diagnosis
4. Additional tips
Good presentation skills are required of the case presenter and the case discussant. The participants must be well prepared and well rehearsed. The time of each segment of the CPC is restricted. Always adhere to the time limits set for the competition. Speakers must be dressed appropriately and present themselves in a professional manner.
Avoid crowded PowerPoint slides, spelling errors, irrelevant artwork, and distracting color schemes. Points are assigned for slide quality, so spend some time on format and arrangement!
Be engaging and enthusiastic. Avoid monotonous speech, mumbling, distracting mannerisms, meaningless phrases and interjections, and a motionless presentation. Humor may be a useful adjunct to the presentation but is used with caution. Have fun, but do not tell inappropriate jokes that might offend members of the audience.
CHECK YOUR EMAILS REGULARLY SPAM AND INBOX FOR QUERIES AND COMMUNICATIONS FROM AND WITH THE JUDGES.
YOU CANNOT WITHHOLD ANY INORMATION WHEN YOU SUBMIT THE CASE SUBMIT ALL THE DATA WITH DAIGNOSIS: THERE HAS TO BE ONE DAIGNOSIS JUDGES WILL HAVE RIGHT TO AUDIT YOUR DATA